氟哌啶醇
 | |
 | |
| 临床资料 | |
|---|---|
| 读音 | /ˌhæloʊˈpɛrɪdɒl/ |
| 商品名 | Haldol及其他 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682180 |
| 核准状况 | |
| 怀孕分级 | |
| 给药途径 | 口服给药, 肌肉注射, 静脉注射, 储库注射 (如癸酸酯制剂,能够缓慢释放药物(长效制剂),而能减少用药频率。) |
| 药物类别 | 典型抗精神病药物 |
| ATC码 | |
| 法律规范状态 | |
| 法律规范 |
|
| 药物动力学数据 | |
| 生物利用度 | 60–70% (口服)[2] |
| 血浆蛋白结合率 | ~90%[2] |
| 药物代谢 | 肝脏介导[2] |
| 代谢产物 | • HPP+[3][4][5] |
| 生物半衰期 | 14–26小时 (静脉注射), 20.7小时 (肌肉注射), 14–37小时 (口服)[2] |
| 排泄途径 | 胆管 (而进入粪便) 及尿液[2][6] |
| 识别信息 | |
| |
| CAS号 | 52-86-8 |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.142 |
| 化学信息 | |
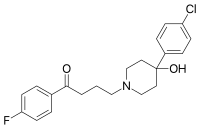
| 化学式 | C21H23ClFNO2 |
| 摩尔质量 | 375.87 g·mol−1 |
| 3D模型(JSmol) | |
| |
| |
氟哌啶醇(INN:haloperidol)以好度(Haldol)等商品名称于市场上贩售,是一种典型抗精神病药物(又称第一代抗精神药物)。[8]用于治疗思觉失调症、妥瑞氏症的抽动症状、双向障碍的躁狂、谵妄、激动、急性精神病和酒精戒断症候群引起的幻觉。[8][9][10]给药方式有口服,肌肉注射或是静脉注射。[8]用药后通常在30至60分钟内发生作用。[8]有每隔4周注射一次的长效药剂(癸酸酯制剂),供患有思觉失调症或相关疾病的人使用,这类人会忘记或拒绝以口服方式用药。[8]
使用氟哌啶醇可能会导致一种称为迟发性运动不能的疾患,且可能是永久性。[8]使用后可能发生神经阻滞剂恶性综合征和心电图中QT间期延长,后者尤其会在静脉注射后发生。[8]此药物在患有失智症的老人中会导致死亡风险升高。[8]个体于怀孕期间服用可能会导致胎儿出现问题。[8][11]罹患帕金森氏症的个体不应使用。[8]
氟哌啶醇于1958年由比利时药学家保罗·杨森领导的团队发现,[12]是从哌替啶(镇痛药)衍生而来的一种药物。[13]它已列入世界卫生组织基本药物标准清单之中,[14]氟哌啶醇是最常使用的典型抗精神病药物,[15]是美国于2020年排名第303的最常使用处方药,开立的处方笺数量超过100万份。[16]
医疗用途
[编辑]氟哌啶醇用于控制下列症状:
- 急性精神病,例如由氯胺酮和苯环己哌啶引起的药物诱发性精神病。[17][18]
- 酒精和阿片类药物戒断的辅助治疗
- 与大脑硬化相关的激动和混乱
- 酒精诱发的精神病
- 酒精戒断症候群所致的幻觉[9]
- 过动性谵妄
- 过动/攻击行为
- 儿童和青少年难以控制的严重行为障碍
- 思觉失调症[19]
- 人格障碍的治疗试验
- 难治性打嗝的治疗[20][21]
- 神经系统疾患的治疗
- 手术后和缓和疗护中的严重恶心和呕吐的治疗
- 作为急性精神科护理中的药物辅助控制[22]
氟哌啶醇虽然曾是精神科急症治疗的主力药物,[22][23]但根据2001年至2005年间发表的多项共识评审,非典型药物在近年来已逐渐取代其地位,成为许多临床治疗的优先选择。[24][25][26]
一项于2013年所做的研究,比较15种抗精神病药物于治疗思觉失调症的疗效,显示氟哌啶醇表现出标准的治疗效果。氟哌啶醇的有效性比齐拉西酮、氯丙嗪和阿塞纳平高出13-16%,与喹硫平、阿立哌唑的效果相当,但比帕利哌酮略差10%。[27]
氟哌啶醇与与某些抗精神病药物(如利培酮)不同,对于血清素迷幻药物(如赛洛西宾(又称裸盖菇素)和麦角酸二乙酰胺(LSD))并无作为解药或是"幻觉终结者"的作用。[28][29][30]
怀孕与母乳哺育期间使用
[编辑]有孕妇使用后可能导致胎儿损害的报告,但此类妇女大多数在怀孕期间接触过多种药物,且目前尚无人类使用的对照研究。根据公认的一般原则,只有在对母亲的益处明显大于对胎儿的潜在风险时,才可在怀孕期间使用此药物。[19]
氟哌啶醇会分泌到母乳中。有几项研究关于此对母乳哺育婴儿的影响,尚未发现对其生长发育有不良影响。[31]
其他应注意处
[编辑]
为维持疾病缓解而长期使用氟哌啶醇治疗慢性精神疾病的患者,应将每日剂量逐步降低至最低有效剂量。在某些情况下,可能会在最终停药。[32]建议在长期使用期间进行常规监测,包括测量身体质量指数、血压、空腹血糖和血脂,以降低副作用导致的风险。[33]
氟哌啶醇的外用药物制剂不应被用于治疗恶心,因为研究表明这种疗法并没有比其他方法更为有效。[34]
不良反应
[编辑]根据一项于2013年对15种抗精神病药物进行比较疗效和耐受性的统合分析,氟哌啶醇是最易引起锥体外症候群副作用的药物之一。[27]
使用超过6个月后,有14%的使用者会增加体重。[35]氟哌啶醇可能具有神经毒性。[36]
如果长期服用这种药物,可能会产生心理上的依赖。[37]
禁忌症
[编辑]药物交互作用
[编辑]氟哌啶醇会与下列药物发生各式交互作用:
潜在神经毒性
[编辑]停药
[编辑]英国国家处方集建议在停用抗精神病药物时采逐步减量方式,以避免急性戒断症候群或快速复发。[41]戒断症状通常有恶心、呕吐和食欲减退。[42]其他症状有焦躁不安、出汗增加和睡眠困难。[42]
药物过量
[编辑]处理
[编辑]主要是对症治疗,包括加强监测生命体征,特别是针对QT间期延长,并对严重心律不整采取抗心律不整措施。[19]
预后
[编辑]氟哌啶醇过量有高致死率风险,[43]但个体经积极治疗后的存活率可望提高。
药理学
[编辑]
氟哌啶醇是一种常见的精神科用药,属于丁酰苯类抗精神病药。它能有效阻断大脑中的多巴胺D2受体,并长时间停留在受体上,达到治疗的效果。[44]它的作用机制与另一类药物啡噻嗪相似。[21]
药物动力学
[编辑]口服
[编辑]氟哌啶醇的口服剂生物利用度介于60%至70%之间。然而,不同研究报告的平均Tmax(达到峰值浓度时间)和T1/2(生物半衰期)差异很大,分别从1.7至6.1小时和14.5至36.7小时不等。[2]
肌内注射
[编辑]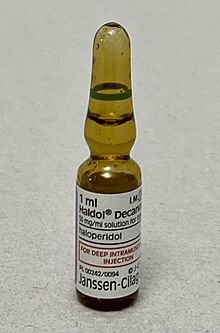
药物经肌内注射后可被快速且完全吸收,具有高生物利用度。健康个体的Tmax(为20分钟,思觉失调症患者为33.8分钟。平均T1/2为20.7小时。[2]长效的氟哌啶醇奎酸酯注射剂仅供肌内注射用,不可进行静脉注射。此针剂于注射后约6天可达血浆峰值浓度,随后浓度下降,生物半衰期约为3周。[46]
静脉注射
[编辑]静脉注射剂的生物利用度为100%,且极快发生作用(仅需数秒)。T1/22为14.1至26.2小时。表观分布容积为9.5至21.7升/公斤。[2]作用持续时间为4至6小时。
化学
[编辑]氟哌啶醇是一种晶体物质,熔点为150°C。[47]晶体在水中的溶解度非常低(1.4毫克/100毫升100),但可溶于氯仿、苯、甲醇和丙酮。它也可溶于0.1摩尔盐酸(3毫克/毫升),但需加热。[48]
历史
[编辑]氟哌啶醇由保罗·杨森领带的团队发现,[49]于1958年在保罗·杨森所创的杨森制药开发,并于同年较晚时在比利时进行首次临床试验。[50][51]
此药物于1967年4月12日获得美国食品药物管理局(FDA)批准,后来由McNeil Laboratories以Haldol(静脉注射剂)品牌名称在美国和其他国家销售。[50]
社会与文化
[编辑]成本
[编辑]氟哌啶醇的价格优势极为突出,较新型抗精神病药物便宜近一百倍,使其成为经济相对弱势患者的更佳选择。[52][53]
名称
[编辑]Haloperidol 是国际非专有药名(INN)、英国批准名称 (BAN)、美国采用名称(USAN)和澳大利亚批准名称(AAN)所认可的名称。
Haloperidol 在全球各地以不同的商品名销售,包括 Aloperidin、Bioperidolo、Brotopon、Dozic、Duraperidol (德国)、Einalon S、Eukystol、Haldol、Halosten、Keselan、Linton、Peluces、Serenace、Serenase及Sigaperidol。[54]
研究
[编辑]氟哌啶醇曾被研究用于治疗忧郁症,[55][56]其机制为: 透过短暂阻断多巴胺受体,大脑会产生一种补偿性反应,增加多巴胺受体的数量,提高对多巴胺的敏感性。当停药后,这种增强的敏感性有助于改善忧郁症状。[55][57][56]
兽医用途
[编辑]氟哌啶醇不仅限于人类医疗,在动物管理,尤其是兽医诊疗和圈养动物管理中,常被用于达到镇静和降低行为激动的效果。[58]
参考文献
[编辑]- ^ Haloperidol Use During Pregnancy. Drugs.com. 2020-02-10 [2020-09-13].
- ^ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Kudo S, Ishizaki T. Pharmacokinetics of haloperidol: an update. Clinical Pharmacokinetics. December 1999, 37 (6): 435–456. PMID 10628896. S2CID 71360020. doi:10.2165/00003088-199937060-00001.
- ^ Kostrzewa RM. Survey of Selective Monoaminergic Neurotoxins Targeting Dopaminergic, Noradrenergic, and Serotoninergic Neurons. Handbook of Neurotoxicity. Cham: Springer International Publishing. 2022: 159–198. ISBN 978-3-031-15079-1. doi:10.1007/978-3-031-15080-7_53.
- ^ Igarashi, Kazuo. The Possible Role of an Active Metafbollte Derived from the Neuroleptic Agent Haloperidol in Drug-Induced Parkinsonism. Journal of Toxicology: Toxin Reviews. 1998, 17 (1): 27–38. ISSN 0731-3837. doi:10.3109/15569549809006488.
- ^ Górska A, Marszałł M, Sloderbach A. Neurotoksyczność pirydyniowych metabolitów haloperydolu [The neurotoxicity of pyridinium metabolites of haloperidol]. Postepy Hig Med Dosw (Online). October 2015, 69: 1169–1175. PMID 26561842. doi:10.5604/17322693.1175009
 (不活跃 2024-11-01) (Polish).
(不活跃 2024-11-01) (Polish).
- ^ Product Information Serenace (PDF). TGA eBusiness Services. Aspen Pharma Pty Ltd. 2011-09-29 [2014-05-29]. (原始内容存档于2017-03-14).
- ^ Anvisa. RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control]. Diário Oficial da União. 2023-03-31 (2023-04-04) [2023-08-16]. (原始内容存档于2023-08-03) (巴西葡萄牙语).
- ^ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 Haloperidol. The American Society of Health-System Pharmacists. [2015-01-02]. (原始内容存档于2015-01-02).
- ^ 9.0 9.1 Schuckit MA. Recognition and management of withdrawal delirium (delirium tremens). The New England Journal of Medicine. November 2014, 371 (22): 2109–2113. PMID 25427113. S2CID 205116954. doi:10.1056/NEJMra1407298.
- ^ Plosker GL. Quetiapine: a pharmacoeconomic review of its use in bipolar disorder. PharmacoEconomics. July 2012, 30 (7): 611–631. PMID 22559293. doi:10.2165/11208500-000000000-00000.
- ^ Prescribing medicines in pregnancy database. Australian Government. 2014-03-03 [2015-01-02]. (原始内容存档于2014-04-08).
- ^ Sneader W. Drug discovery : a history Rev. and updated. Chichester: Wiley. 2005: 124. ISBN 978-0-471-89979-2. (原始内容存档于2015-12-08).
- ^ Ravina E. The evolution of drug discovery: from traditional medicines to modern drugs 1. Aufl. Weinheim: Wiley-VCH. 2011: 62. ISBN 978-3-527-32669-3. (原始内容存档于2015-12-08).
- ^ World Health Organization. World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. hdl:10665/345533
 . WHO/MHP/HPS/EML/2021.02.
. WHO/MHP/HPS/EML/2021.02.
- ^ Stevens A. Health care needs assessment: the epidemiologically based needs assessment reviews 2nd. Abingdon: Radcliffe Medical. 2004: 202. ISBN 978-1-85775-892-4. (原始内容存档于2015-12-08).
- ^ Haloperidol - Drug Usage Statistics. ClinCalc. [2022-10-07].
- ^ Giannini AJ, Underwood NA, Condon M. Acute ketamine intoxication treated by haloperidol: a preliminary study. American Journal of Therapeutics. November 2000, 7 (6): 389–391. PMID 11304647. doi:10.1097/00045391-200007060-00008.
- ^ Giannini AJ, Eighan MS, Loiselle RH, Giannini MC. Comparison of haloperidol and chlorpromazine in the treatment of phencyclidine psychosis. Journal of Clinical Pharmacology. April 1984, 24 (4): 202–204. PMID 6725621. S2CID 42278510. doi:10.1002/j.1552-4604.1984.tb01831.x.
- ^ 19.0 19.1 19.2 Haldol Official FDA information, side effects and uses. Drugs.com. [2013-10-03]. (原始内容存档于2013-10-05).
- ^ Joint Formulary Committee. British National Formulary (BNF) 65th. London, England: Pharmaceutical Press. 2013: 229–30. ISBN 978-0-85711-084-8.
- ^ 21.0 21.1 Brayfield, A (编). Haloperidol. Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. 2013 -12-13 [2014-05-29].
- ^ 22.0 22.1 Currier GW. The controversy over "chemical restraint" in acute care psychiatry. Journal of Psychiatric Practice (Lippincott Williams & Wilkins). January 2003, 9 (1): 59–70. PMID 15985915. S2CID 22342074. doi:10.1097/00131746-200301000-00006.
- ^ Cavanaugh SV. Psychiatric emergencies. The Medical Clinics of North America. September 1986, 70 (5): 1185–1202. PMID 3736271. doi:10.1016/S0025-7125(16)30919-1.
- ^ Allen MH, Currier GW, Hughes DH, Reyes-Harde M, Docherty JP. The Expert Consensus Guideline Series. Treatment of behavioral emergencies. Postgraduate Medicine. May 2001, (Spec No): 1–88; quiz 89–90. PMID 11500996.
- ^ Allen MH, Currier GW, Hughes DH, Docherty JP, Carpenter D, Ross R. Treatment of behavioral emergencies: a summary of the expert consensus guidelines. Journal of Psychiatric Practice. January 2003, 9 (1): 16–38. PMID 15985913. S2CID 29363701. doi:10.1097/00131746-200301000-00004.
- ^ Allen MH, Currier GW, Carpenter D, Ross RW, Docherty JP. The expert consensus guideline series. Treatment of behavioral emergencies 2005. Journal of Psychiatric Practice. November 2005, 11 (Suppl 1): 5–25. PMID 16319571. S2CID 72366588. doi:10.1097/00131746-200511001-00002.
- ^ 27.0 27.1 Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. September 2013, 382 (9896): 951–962. PMID 23810019. S2CID 32085212. doi:10.1016/S0140-6736(13)60733-3.
- ^ Halman A, Kong G, Sarris J, Perkins D. Drug-drug interactions involving classic psychedelics: A systematic review. J Psychopharmacol. January 2024, 38 (1): 3–18. PMC 10851641
 . PMID 37982394. doi:10.1177/02698811231211219.
. PMID 37982394. doi:10.1177/02698811231211219.
- ^ Halberstadt AL. Recent advances in the neuropsychopharmacology of serotonergic hallucinogens. Behav Brain Res. January 2015, 277: 99–120. PMC 4642895
 . PMID 25036425. doi:10.1016/j.bbr.2014.07.016.
. PMID 25036425. doi:10.1016/j.bbr.2014.07.016.
- ^ Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Bäbler A, Vogel H, Hell D. Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. NeuroReport. December 1998, 9 (17): 3897–3902. PMID 9875725. doi:10.1097/00001756-199812010-00024.
- ^ LACTMED: Haloperidol. 2018-10-31 [2019-01-18].
- ^ Haloperidol. CHEMEUROPE.com. [2024--12-14].
- ^ Work Group on Schizophrenia. Practice Guideline for the Treatment of Patients With Schizophrenia Second. [2014-04-21]. (原始内容存档于2012-03-27).
- ^ American Academy of Hospice and Palliative Medicine. Five Things Physicians and Patients Should Question. Choosing Wisely: An Initiative of the ABIM Foundation (American Academy of Hospice and Palliative Medicine). [2013-08-01]. (原始内容存档于2013-09-01)., which cites
- Smith TJ, Ritter JK, Poklis JL, Fletcher D, Coyne PJ, Dodson P, Parker G. ABH gel is not absorbed from the skin of normal volunteers. Journal of Pain and Symptom Management. May 2012, 43 (5): 961–966. PMID 22560361. doi:10.1016/j.jpainsymman.2011.05.017
 .
. - Weschules DJ. Tolerability of the compound ABHR in hospice patients. Journal of Palliative Medicine. December 2005, 8 (6): 1135–1143. PMID 16351526. doi:10.1089/jpm.2005.8.1135.
- Smith TJ, Ritter JK, Poklis JL, Fletcher D, Coyne PJ, Dodson P, Parker G. ABH gel is not absorbed from the skin of normal volunteers. Journal of Pain and Symptom Management. May 2012, 43 (5): 961–966. PMID 22560361. doi:10.1016/j.jpainsymman.2011.05.017
- ^ FDA Psychopharmacological Drugs Advisory Committee. Briefing Document for ZELDOX CAPSULES (Ziprasidone HCl) (PDF). Food and Drug Administration. 2000-07-09 [2016-09-30]. (原始内容 (PDF)存档于2017-01-19).
- ^ Nasrallah HA, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Annals of Clinical Psychiatry. August 2017, 29 (3): 195–202. PMID 28738100.
- ^ Haloperidol Withdrawal Symptoms: An Overview.
- ^ Sattler, Stefan M; Lubberding, Anniek F. Effect of the antipsychotic drug haloperidol on arrhythmias during acute myocardial infarction in a porcine model. IJC Heart & Vasculature. 2019-12-30, 26 (100455) [2024-12-15]. doi:10.1016/j.ijcha.2019.100455.
- ^ Nasrallah HA, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Annals of Clinical Psychiatry. August 2017, 29 (3): 195–202. PMID 28738100.
- ^ Pierre JM. Time to retire haloperidol?. Current Psychiatry: 19.
- ^ Joint Formulary Committee, BMJ (编). 4.2.1. British National Formulary 57. United Kingdom: Royal Pharmaceutical Society of Great Britain. March 2009: 192. ISBN 978-0-85369-845-6.
Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.
- ^ 42.0 42.1 Haddad PM, Dursun S, Deakin B. Adverse Syndromes and Psychiatric Drugs: A Clinical Guide. OUP Oxford. 2004: 207–216. ISBN 9780198527480 (英语).
- ^ Haloperidol at Drugs.com. (原始内容存档于2011-11-22).
- ^ Seeman P, Tallerico T. Antipsychotic drugs which elicit little or no parkinsonism bind more loosely than dopamine to brain D2 receptors, yet occupy high levels of these receptors. Molecular Psychiatry. March 1998, 3 (2): 123–134. PMID 9577836. doi:10.1038/sj.mp.4000336
 .
.
- ^ Haldol Decanoate - Summary of Product Characteristics (SmPC) - (emc). www.medicines.org.uk. [2021-12-26].
- ^ drugs.com. (原始内容存档于2011-08-10).
- ^ Shan X, Williams AC, Khutoryanskiy VV. Polymer structure and property effects on solid dispersions with haloperidol: Poly(N-vinyl pyrrolidone) and poly(2-oxazolines) studies (PDF). International Journal of Pharmaceutics. November 2020, 590: 119884. PMID 32950665. S2CID 221826541. doi:10.1016/j.ijpharm.2020.119884.
- ^ Sigma data sheet on haloperidol (PDF).
- ^ Healy D. The psychopharmacologists 1. London: Chapman and Hall. 1996. ISBN 978-1-86036-008-4.[页码请求]
- ^ 50.0 50.1 Granger B, Albu S. The haloperidol story. Annals of Clinical Psychiatry. 2005, 17 (3): 137–140. PMID 16433054. doi:10.1080/10401230591002048.
- ^ López-Muñoz F, Alamo C. The consolidation of neuroleptic therapy: Janssen, the discovery of haloperidol and its introduction into clinical practice. Brain Research Bulletin. April 2009, 79 (2): 130–141. PMID 19186209. S2CID 7720401. doi:10.1016/j.brainresbull.2009.01.005.
- ^ Escobar JI, Marin H. Clinical Psychopharmacology: A Practical Approach. World Scientific. 2013: 69. ISBN 978-981-4578-37-0 (英语).
- ^ Adams JG. Emergency Medicine E-Book: Clinical Essentials (Expert Consult -- Online). Elsevier Health Sciences. 2012: 1635. ISBN 978-1-4557-3394-1 (英语).
- ^ Haloperidol. Hölzel. [2024-12-14].
- ^ 55.0 55.1 CLR 3001. AdisInsight. 27 August 2019 [13 August 2024].
- ^ 56.0 56.1 Kennedy SH, Giacobbe P, Placenza F, Hudson CJ, Seeman P, Seeman MV. Depression treatment by withdrawal of short-term low-dose antipsychotic, a proof-of-concept randomized double-blind study. J Affect Disord. September 2014, 166: 139–143. PMID 25012422. doi:10.1016/j.jad.2014.04.014.
- ^ Cohen D, Recalt A. Discontinuing Psychotropic Drugs from Participants in Randomized Controlled Trials: A Systematic Review. Psychother Psychosom. 2019, 88 (2): 96–104. PMID 30923288. doi:10.1159/000496733.
- ^ Hofmeyr JM. The use of haloperidol as a long-acting neuroleptic in game capture operations. Journal of the South African Veterinary Association. December 1981, 52 (4): 273–282. PMID 6122740.
