激素宫内节育器
| 激素宫内节育器 | |
|---|---|
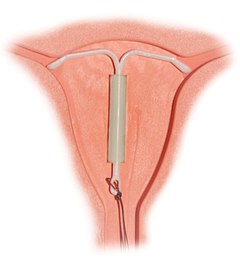 正确置入的宫内节育器 | |
| 背景 | |
| 生育控制种类 | 宫内节育器 |
| 初次使用日期 | 1990 (Mirena—现仍在使用) 1976 (Progestasert—于2001停用) |
| 失败比率 (置入后第一年) | |
| 完美使用 | 0.1–0.2% |
| 一般使用 | 0.1–0.2% |
| 用法 | |
| 持续期间 | 3–8年 |
| 可逆性 | 2–6月 |
| 注意事项 | 每月检查线绳位置 |
| 医师诊断 | 一个月后复查,此后每年至少复查一次 |
| 优点及缺点 | |
| 是否可以防止性传播疾病 | 否 |
| 周期 | 月经不规则,经血通常较少,或无月经 |
| 是否影响体重 | 可能的副作用 |
| 好处 | 无需每日采取避孕腊施 |
| 风险 | 良性卵巢囊肿、骨盆腔发炎、子宫穿孔(罕见)等 |
激素宫内节育器(hormonal intrauterine device)常见者为含孕激素子宫内系统(intrauterine system (IUS) with progestogen),商品名有 Mirena(蜜蕊娜、曼月乐)等,是一种可以释放激素(如属于孕激素的左炔诺孕酮)的宫内节育器[1],其用途包括避孕、缓解月经过多、预防雌激素替代疗法可能产生的子宫内膜增生等[1]。
含孕激素IUD是最有效的避孕方法之一,年避孕失败率约为0.2%[2]。该装置经由手术放入子宫中,有效期为3到8年[3][4]。取出之后,生育能力将很快恢复[1]。
使用此装置的副作用有经期不规则、良性卵巢囊肿、骨盆腔疼痛和忧郁[1]。罕见案例有子宫穿孔[1]。不建议个体于怀孕期间使用,但母乳哺育期间使用对于婴儿属于安全[1]。含孕激素IUD是一种长效且可逆的避孕方法[5]。作用机制是通过孕激素以稠化宫颈黏液并让子宫内膜变薄,从而抑制精子通过宫颈并影响受精卵着床,偶尔也会抑制排卵,借由这些机制起到避孕的作用[1]。
含左炔诺孕酮的IUD于1990年在芬兰首次获准用于医疗用途,并于2000年获准在美国使用[6]。此装置已列入世界卫生组织基本药物标准清单之中[7][8]。
医疗用途
[编辑]| 临床资料 | |
|---|---|
| 怀孕分级 | |
| ATC码 |
|
| 法律规范状态 | |
| 法律规范 |
|
含孕激素IUD是一种极其有效的避孕方法,于2021年所做的一项研究显示它可用于紧急避孕[15]。含孕激素IUD除用于避孕之外,还用于预防和治疗:
- 经血过多[16]
- 子宫内膜异位症和慢性骨盆腔疼痛[16][17]
- 子宫腺肌病和经痛[16][18]
- 贫血[19]
- 子宫内膜增生症(特别是对希望在治疗子宫内膜增生症的同时仍保持生育能力的更年期前女性)[20][21]
- 在某些情况下,使用含孕激素IUD可避免进行子宫切除术[22]。
优点:
- 为最有效且可逆的避孕法之一[23]
- 个体于母乳哺育期间可使用[24]
- 无性行为前准备事项,[25]但建议用者和医师定期检查装置的线绳,以确保其位置正确[26]
- 希望再度怀孕的用者在移除装置后的24个月内有90%能成功怀孕[27]
- 可能经血变少(有些女性的月经甚至完全停止)[28]
- 有效期长达3至8年(依含孕激素IUD种类而异)[4]
缺点:
有效性
[编辑]使用商品名为Mirena的装置可有效避孕长达8年[29]。使用商品名为Kyleena的装置,有效期为5年,而使用商品名为Skyla的装置,有效期为3年[30][31]。
含孕激素IUD是一种长效且可逆的避孕法,被认为是最有效的避孕方式之一。此装置的第1年失败率为0.1-0.2%,5年失败率为0.7-0.9%[32][29][33]。此类失败率与输卵管结扎技术相当,但不同点是含孕激素IUD的做法为可逆。
含孕激素IUD被认为比其他常见的可逆避孕法(如复合口服避孕药)更有效,因为用者于置入之后几乎不必做任何事[23]。其他避孕法的效果会受到用者本身的作为而降低,如服药时间不准。使用含孕激素IUD后毋须每日、每周或每月服药,因此其典型使用失败率与完美使用失败率相同[23]。
在一项为期10年的研究中,发现使用含左炔诺孕酮IUD在治疗经血过多方面与口服药物(如传明酸、甲芬那酸、雌激素与黄体素复合制剂或单纯孕激素)的效果相当,前述女性未因经血过多而需进行手术,且生活品质仍获得改善[34][35]。
有双角子宫的女性若需避孕,通常会放置两个IUD(每个角一个),因只做单一子宫角放置的避孕效果尚无足够实证支持[36]。目前尚无充分的科学证据支持将含孕激素IUD用于治疗双角子宫个体的经血过多。然而有部分个案报告显示,单一含孕激素IUD在治疗此类个体方面具有一定的疗效。[37]。
母乳哺育
[编辑]含孕激素的避孕方法(例如IUD)被认为不会影响母乳供应或婴儿生长[38]。然而在Mirena申请DA核准的研究中发现使用此种含孕激素IUD的母亲有44%于75天后仍继续哺乳,低于使用铜质IUD的母亲 (79%于75天后仍继续哺乳)[39]。:37
使用Mirena的个体,约有0.1%的左炔诺孕酮会通过母乳传递给哺乳婴儿[40]。一项针对母亲使用单纯左炔诺孕酮避孕法的哺乳婴儿进行的为期6年研究,发现这些婴儿患呼吸道感染和眼部感染的风险较母亲使用铜质IUD的婴儿为高,但神经系统疾病的风险较低[41]。目前尚无任何长期的研究来评估母乳中左炔诺孕酮对婴儿在长期方面的影响。
对于哺乳中的母亲,美国疾病管制与预防中心(CDC)建议激素避孕法并非首选。不过,如果选择使用像Mirena这样仅含孕激素避孕器,建议只有在评估后,认为益处大于风险时才适合使用,在使用期间也须密切观察身体状况[42]。世界卫生组织(WHO)建议避免个体于产后立即置入,理由是装置从子宫脱落的比率会增加。WHO对产后6周内母亲使用Mirena,可能对婴儿肝脏和脑部发育造成的潜在影响表示担忧,并强调需要更多的研究来评估其安全性。然而WHO建议从产后6周开始,即使是哺乳妇女,也可用Mirena作为避孕选项[43][44]。非营利组织美国计划生育联合会则建议可在产后4周即开始为哺乳妇女提供Mirena作为避孕选项[45]。
禁忌症
[编辑]个体有以下的情况即不应使用含孕激素IUD:
- 怀孕中或怀疑已怀孕者[24]
- 有不明原因的异常阴道出血者[24](此点有争议)[46]
- 患有未经治疗的子宫颈癌或子宫癌者[24]
- 患有或可能患有乳癌者[24]
- 子宫颈或子宫异常者[47](此点有争议)[46]
- 近三个月内曾患有骨盆腔发炎者[24]
- 近三个月内曾感染性传染病者(如披衣菌感染或淋病)[24]
- 患有肝病或肿瘤者[47]
- 对左炔诺孕酮或装置中任何非活性成分过敏者[47]
进行子宫扩张与刮除术(D&E)人工流产(中期妊娠终止)后的个体可装置IUD,但可能会增加装置从子宫脱落比率[48]。为降低感染风险,不建议在以下情况下进行IUD置入: 1. 接受药物流产后,尚未进行超声波检查以确认流产已完全。 2. 接受药物流产后,尚未出现第一次月经[45]。
完整的禁忌症清单可在世界卫生组织避孕药物使用医学适应症标准(Medical Eligibility Criteria for Contraceptive Use)和CDC美国避孕药物使用医学适应症标准(United States Medical Eligibility Criteria for Contraceptive Use)中取得[24][49]。
副作用
[编辑]- 经期不规则、[50][51][52]
- 痉挛和疼痛、[53]
- 装置脱落、 [53][54][55][56][57]
- 子宫穿孔、[58][56]
- 怀孕并发症、[39]:3–4[53][54][53][54][39]:5,41
- 感染、[59][53]
- 卵巢囊肿、[60][61]
- 精神健康变化,(包括神经紧张、情绪低落、情绪波动)、[47]
- 体重增加、[47]
- 头痛或偏头痛、[47]
- 恶心、[47]
- 痤疮、[47]
- 毛发过多、[47]
- 下腹或背部疼痛、[47]
- 性欲减退、[47]
- 阴道瘙痒、发红或肿胀、[47]
- 阴道产生分泌物、[62]
- 乳房疼痛、压痛、[62]
- 水肿、[62]
- 腹胀、[62]
- 子宫颈炎、[62]
- 细菌性阴道病、[63]
- 可能会影响葡萄糖耐受性、[62]
- 可能会出现视力变化或隐形眼镜耐受性改变、[27]
- 可能会导致维生素B1缺乏,影响精力、情绪和神经系统功能、[27]
- "线绳消失" - 指妇女在例行检查时无法触摸到IUD的线绳,且在膣镜检查下也无法看到[64][65]。
癌症
[编辑]根据国际癌症研究机构 (IARC) 于1999年对仅含孕激素避孕法进行的评估,有一些证据显示此避孕法可降低子宫内膜癌的风险。IARC于1999年的研究结论,表示没证据表明仅含孕激素的避孕法会增加任何癌症的风险,但所做研究的规模太小,无法取得确定结论[66]。
骨质密度
[编辑]没证据显示Mirena会影响用者的骨质密度[67]。两项针对前臂骨质的小型研究显示密度并下降[68][69]。
组成与激素释放
[编辑]
含孕激素IUD是一种小的T形塑料装置,含有左炔诺孕酮,[29]微量左炔诺孕酮会逐步释放进入子宫(主要是旁分泌,而非全身性),其中大部分留在子宫内,有少量会进入身体其他部位[53]。
置入与移除IUD
[编辑]图片说明(由左至右):
1. 将MirenaIUD置入阴道的超声波扫描示意图。
2. 置入含孕激素IUD
3. 移除含孕激素IUD
作用机转
[编辑]左炔诺孕酮是一种孕激素受体激动剂。最新的研究显示含孕激素IUD的主要避孕机制是防止卵子受精[53][70][71][72][73]
历史
[编辑]
铜质IUD在1960年代和1970年代开发上市,而含孕激素IUD于1970年代开发成功[74]。于芝加哥迈克尔·里斯医院服务的安东尼奥·斯科门加医生(Dr. Antonio Scommenga)发现,在子宫内施用孕酮具有避孕功效[74]。芬兰医生约尼·瓦尔特·塔帕尼·卢卡伊宁根据安东尼奥·斯科门加医生的发现而制造可释放孕酮的T形IUD,于1976年以Progestasert System商品名称上市。第一代子宫内避孕器使用寿命很短,只有1年,市场表现不佳。卢卡伊宁医生后来改用左炔诺孕酮,研发出可持续使用5年的Mirena,大幅提升避孕器的效用[75]。
FDA于2013年核准商品名称为Skyla的避孕器上市(为一种有效期长达3年的低剂量左炔诺孕酮IUD)[76]。Skyla造成的月经模式与Mirena不同,临床试验中,使用Skyla者只有6%出现闭经(而使用Mirena者约有20%会出现)。
目前Mirena避孕器系列仅在芬兰生产[77]。
争议
[编辑]Mirena的制造商拜耳公司因夸大产品功效、淡化使用风险以及对该装置进行"虚假或误导性陈述"而收到美国食品药物管理局警告信[78][79]。美国联邦机构在2000年到2013年期间收到超过70,072份关于该装置和相关不良反应的投诉[80][81]。截至2014年4月,美国已有超过1,200件对此装置兴起的法律诉讼[79][82][83][84]。
参考文献
[编辑]- ^ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 British National Formulary: BNF 69 69th. British Medical Association. 2015: 556. ISBN 978-0-85711-156-2.
- ^ 引用错误:没有为名为
Trus2011的参考文献提供内容 - ^ Levonorgestrel intrauterine system medical facts from Drugs.com. drugs.com. [2017-01-01]. (原始内容存档于2017-01-01).
- ^ 4.0 4.1 4.2 Hormonal IUDs. www.plannedparenthood.org. [2019-04-20]. (原始内容存档于2019-04-24) (英语).
- ^ Wipf J. Women's Health, An Issue of Medical Clinics of North America. Elsevier Health Sciences. 2015: 507 [2017-09-01]. ISBN 978-0-323-37608-2. (原始内容存档于2023-01-10).
- ^ Bradley LD, Falcone T. Hysteroscopy: Office Evaluation and Management of the Uterine Cavity. Elsevier Health Sciences. 2008: 171 [2017-09-01]. ISBN 978-0-323-04101-0. (原始内容存档于2023-1-12).
- ^ World Health Organization. World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. hdl:10665/325771
 . WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ World Health Organization. World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. hdl:10665/345533
 . WHO/MHP/HPS/EML/2021.02.
. WHO/MHP/HPS/EML/2021.02.
- ^ 9.0 9.1 Mirena (levonorgestrel) intrauterine device. Therapeutic Goods Administration (TGA). 2024-07-17 [2024-10-12].
- ^ Mirena Product information. Health Canada. 2007-11-22 [2024-04-19]. (原始内容存档于2024-04-19).
- ^ Mirena - levonorgestrel intrauterine device. Bayer Health Pharmaceuticals. May 2009 [18 June 2015]. (原始内容存档于18 June 2015).
- ^ Kyleena- levonorgestrel intrauterine device. DailyMed. 13 March 2023 [2024-04-19]. (原始内容存档于2023-09-22).
- ^ Skyla- levonorgestrel intrauterine device. DailyMed. 2023-01-31 [2024 -04-19]. (原始内容存档于2023-12-09).
- ^ Liletta- levonorgestrel intrauterine device. DailyMed. 2023-06-29 [2024-04-19]. (原始内容存档于2021-11-29).
- ^ Science Update: Hormonal IUD as effective as a copper IUD at emergency contraception and with less discomfort, NICHD-funded study suggests. 4 February 2021 [2021-07-06]. (原始内容存档于2021-07-26).
- ^ 16.0 16.1 16.2 Bahamondes L, Bahamondes MV, Monteiro I. Levonorgestrel-releasing intrauterine system: uses and controversies. Expert Review of Medical Devices. July 2008, 5 (4): 437–445. PMID 18573044. S2CID 659602. doi:10.1586/17434440.5.4.437.
- ^ Petta CA, Ferriani RA, Abrao MS, Hassan D, Rosa E, Silva JC, Podgaec S, Bahamondes L. Randomized clinical trial of a levonorgestrel-releasing intrauterine system and a depot GnRH analogue for the treatment of chronic pelvic pain in women with endometriosis. Human Reproduction. July 2005, 20 (7): 1993–1998. PMID 15790607. doi:10.1093/humrep/deh869
 .
.
- ^ Sheng J, Zhang WY, Zhang JP, Lu D. The LNG-IUS study on adenomyosis: a 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis. Contraception. March 2009, 79 (3): 189–193. PMID 19185671. doi:10.1016/j.contraception.2008.11.004.
- ^ Faundes A, Alvarez F, Brache V, Tejada AS. The role of the levonorgestrel intrauterine device in the prevention and treatment of iron deficiency anemia during fertility regulation. International Journal of Gynaecology and Obstetrics. June 1988, 26 (3): 429–433. PMID 2900174. S2CID 34592937. doi:10.1016/0020-7292(88)90341-4.
- ^ The American College of Obstetricians and Gynecologists Committee Opinion no. 631. Endometrial intraepithelial neoplasia. Obstetrics and Gynecology. May 2015, 125 (5): 1272–1278. PMID 25932867. S2CID 46508283. doi:10.1097/01.AOG.0000465189.50026.20.
- ^ Mittermeier T, Farrant C, Wise MR. Levonorgestrel-releasing intrauterine system for endometrial hyperplasia. The Cochrane Database of Systematic Reviews. September 2020, 2020 (9): CD012658. PMC 8200645
 . PMID 32909630. doi:10.1002/14651858.CD012658.pub2.
. PMID 32909630. doi:10.1002/14651858.CD012658.pub2.
- ^ Marjoribanks J, Lethaby A, Farquhar C. Surgery versus medical therapy for heavy menstrual bleeding. The Cochrane Database of Systematic Reviews. January 2016, 2016 (1): CD003855. PMC 7104515
 . PMID 26820670. doi:10.1002/14651858.CD003855.pub3.
. PMID 26820670. doi:10.1002/14651858.CD003855.pub3.
- ^ 23.0 23.1 23.2 Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, Secura GM. Effectiveness of long-acting reversible contraception. The New England Journal of Medicine. May 2012, 366 (21): 1998–2007 [2019-06-30]. PMID 22621627. S2CID 16812353. doi:10.1056/NEJMoa1110855
 . (原始内容存档于2020-06-11). 已忽略未知参数
. (原始内容存档于2020-06-11). 已忽略未知参数|df=(帮助) - ^ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, Simmons KB, Pagano HP, Jamieson DJ, Whiteman MK. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016 (PDF). MMWR. Recommendations and Reports. July 2016, 65 (3): 1–103 [2020-02-03]. PMID 27467196. doi:10.15585/mmwr.rr6503a1
 . (原始内容存档 (PDF)于2020-10-16).
. (原始内容存档 (PDF)于2020-10-16).
- ^ IUD. Planned Parenthood. [2015-06-18]. (原始内容存档于2015-06-18).
- ^ Convenience. Let's Talk About Mirena. Bayer. [2015-06-18]. (原始内容存档于2015-06-18).
- ^ 27.0 27.1 27.2 Mirena. MediResource Inc. [2015-06-18]. (原始内容存档于2015-07-03).
- ^ 28.0 28.1 Hidalgo M, Bahamondes L, Perrotti M, Diaz J, Dantas-Monteiro C, Petta C. Bleeding patterns and clinical performance of the levonorgestrel-releasing intrauterine system (Mirena) up to two years. Contraception. February 2002, 65 (2): 129–132. PMID 11927115. doi:10.1016/s0010-7824(01)00302-x.
- ^ 29.0 29.1 29.2 Mirena IUD Homepage | Official Website. [2012-07-19]. (原始内容存档于2012-07-31)., Bayer Pharmaceuticals.
- ^ Highlights of Prescribing Information (报告). 2013-01-09. (原始内容存档于2016-05-06). 已忽略未知参数
|df=(帮助) - ^ What are hormonal IUDs?. Planned Parenthood. [2019-04-19]. (原始内容存档于2019-04-24).
- ^ Westhoff CL, Keder LM, Gangestad A, Teal SB, Olariu AI, Creinin MD. Six-year contraceptive efficacy and continued safety of a levonorgestrel 52 mg intrauterine system. Contraception. March 2020, 101 (3): 159–161 [2 January 2020]. PMID 31786203. S2CID 208535090. doi:10.1016/j.contraception.2019.10.010. (原始内容存档于2020-06-10).
- ^ Jensen JT, Creinin MD, Speroff L (编). Speroff & Darney's clinical guide for contraception Sixth. Philadelphia, PA: Wolters Kluwer. 2019: 15. ISBN 978-1-9751-0728-4. OCLC 1121081247.
- ^ Kai J, Dutton B, Vinogradova Y, Hilken N, Gupta J, Daniels J. Rates of medical or surgical treatment for women with heavy menstrual bleeding: the ECLIPSE trial 10-year observational follow-up study. Health Technology Assessment. October 2023, 27 (17): 1–50 [2024-04-12]. PMC 10641716
 . PMID 37924269. doi:10.3310/JHSW0174. (原始内容存档于2023-11-06) (英语).
. PMID 37924269. doi:10.3310/JHSW0174. (原始内容存档于2023-11-06) (英语).
- ^ The coil and medicines are both effective long-term treatments for heavy periods. NIHR Evidence. 2024-03-08 [2024-04-12]. doi:10.3310/nihrevidence_62335. (原始内容存档于2024-03-18).
- ^ Oelschlager AM, Debiec K, Micks E, Prager S. Use of the Levonorgestrel Intrauterine System in Adolescents With Known Uterine Didelphys or Unicornuate Uterus. Journal of Pediatric and Adolescent Gynecology. 2013, 26 (2): e58. ISSN 1083-3188. doi:10.1016/j.jpag.2013.01.029
 .
.
- ^ Acharya GP, Mills AM. Successful management of intractable menorrhagia with a levonorgestrel-releasing intrauterine device, in a woman with a bicornuate uterus. Journal of Obstetrics and Gynaecology. July 1998, 18 (4): 392–393. PMID 15512123. doi:10.1080/01443619867263.
- ^ Truitt ST, Fraser AB, Grimes DA, Gallo MF, Schulz KF. Lopez LM , 编. Combined hormonal versus nonhormonal versus progestin-only contraception in lactation. The Cochrane Database of Systematic Reviews. 2003, (2): CD003988. PMID 12804497. doi:10.1002/14651858.CD003988.
- ^ 39.0 39.1 39.2 Medical review of NDA 21-225: Mirena (levonorgestrel-releasing intrauterine system) Berlex Laboratories (PDF). Center for Drug Evaluation and Research. U.S. Food and Drug Administration. December 2000. (原始内容 (PDF)存档于2008-02-27).
- ^ MIRENA Data Sheet (PDF). Bayer NZ. 2009-12-11 [2011-02-10]. (原始内容 (PDF)存档于2011-07-06).
- ^ Schiappacasse V, Díaz S, Zepeda A, Alvarado R, Herreros C. Health and growth of infants breastfed by Norplant contraceptive implants users: a six-year follow-up study. Contraception. July 2002, 66 (1): 57–65. PMID 12169382. doi:10.1016/S0010-7824(02)00319-0.
- ^ Classifications for Intrauterine Devices | CDC. www.cdc.gov. 2020-04-09 [2020-07-07]. (原始内容存档于2020-07-15) (美国英语).
- ^ World Health Organization. Medical eligibility criteria for contraceptive use 5th. Geneva: World Health Organization. 2015. ISBN 978-92-4-154915-8. hdl:10665/181468
 .
.
- ^ World Health Organization. Medical eligibility criteria for contraceptive use, fifth edition 2015: executive summary. World Health Organization. 2015 [2020-02-03]. hdl:10665/172915
 . (原始内容存档于2021-08-28).
. (原始内容存档于2021-08-28).
- ^ 45.0 45.1 Understanding IUDs. Planned Parenthood. July 2005 [2006-10-08]. (原始内容存档于2006-10-12).
- ^ 46.0 46.1 Heavy menstrual bleeding (update). National Institute for Health and Care Excellence. 2018.
- ^ 47.00 47.01 47.02 47.03 47.04 47.05 47.06 47.07 47.08 47.09 47.10 47.11 Mirena: Consumer Medicine Information (PDF). Bayer. March 2014 [2014-04-27]. (原始内容存档 (PDF)于2014-04-27).
- ^ Roe AH, Bartz D. Society of Family Planning clinical recommendations: contraception after surgical abortion. Contraception. January 2019, 99 (1): 2–9. PMID 30195718. doi:10.1016/j.contraception.2018.08.016
 .
.
- ^ WHO. Intrauterine devices (IUDs). Medical Eligibility Criteria for Contraceptive Use 4th. Geneva: Reproductive Health and Research, WHO. 2010. ISBN 978-92-4-156388-8. (原始内容存档于2012-07-10).
- ^ Hidalgo M, Bahamondes L, Perrotti M, Diaz J, Dantas-Monteiro C, Petta C. Bleeding patterns and clinical performance of the levonorgestrel-releasing intrauterine system (Mirena) up to two years. Contraception. February 2002, 65 (2): 129–132. PMID 11927115. doi:10.1016/S0010-7824(01)00302-X.
- ^ McCarthy L. Levonorgestrel-Releasing Intrauterine System (Mirena) for Contraception. Am Fam Physician. May 2006, 73 (10): 1799– [4 May 2007]. (原始内容存档于2007-09-26).
- ^ Rönnerdag M, Odlind V. Health effects of long-term use of the intrauterine levonorgestrel-releasing system. A follow-up study over 12 years of continuous use. Acta Obstetricia et Gynecologica Scandinavica. September 1999, 78 (8): 716–721. PMID 10468065. doi:10.1034/j.1600-0412.1999.780810.x
 .
.
- ^ 53.0 53.1 53.2 53.3 53.4 53.5 53.6 Dean G, Schwarz EB. Intrauterine contraceptives (IUCs). Hatcher RA, Trussell J, Nelson AL, Cates Jr W, Kowal D, Policar MS (编). Contraceptive technology 20th revised. New York: Ardent Media. 2011: 147–191. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. p.150:
Mechanism of action
Although the precise mechanism of action is not known, currently available IUCs work primarily by preventing sperm from fertilizing ova.26 IUCs are not abortifacients: they do not interrupt an implanted pregnancy.27 Pregnancy is prevented by a combination of the "foreign body effect" of the plastic or metal frame and the specific action of the medication (copper or levonorgestrel) that is released. Exposure to a foreign body causes a sterile inflammatory reaction in the intrauterine environment that is toxic to sperm and ova and impairs implantation.28,29 The production of cytotoxic peptides and activation of enzymes lead to inhibition of sperm motility, reduced sperm capacite journal and survival, and increased phagocytosis of sperm.30,31… The progestin in the LNg IUC enhances the contraceptive action of the device by thickening cervical mucus, suppressing the endometrium, and impairing sperm function. In addition, ovulation is often impaired as a result of systemic absorption of levonorgestrel.23
p. 162:
Table 7-1. Myths and misconceptions about IUCs
Myth: IUCs are abortifacients. Fact: IUCs prevent fertilization and are true contraceptives. - ^ 54.0 54.1 54.2 IUDs—An Update. Population Reports (Population Information Program, Johns Hopkins School of Public Health). December 1995, XXII (5).
- ^ IUDs—An Update: Chapter 2.7: Expulsion. Population Reports (Population Information Program, Johns Hopkins School of Public Health). December 1995, XXII (5). (原始内容存档于2006-09-05).
- ^ 56.0 56.1 IUDs—An Update: Chapter 3.3: Postpartum Insertion. Population Reports (Population Information Program, Johns Hopkins School of Public Health). December 1995, XXII (5). (原始内容存档于2006-04-29).
- ^ IUDs—An Update: Chapter 3.4: Postabortion Insertion. Population Reports (Population Information Program, Johns Hopkins School of Public Health). December 1995, XXII (5). (原始内容存档于2006-08-11).
- ^ WHO Scientific Group on the Mechanism of Action Safety and Efficacy of Intrauterine Devices, World Health Organization. Mechanism of action, safety and efficacy of intrauterine devices. Geneva: World Health Organization. 1987. ISBN 92-4-120753-1. hdl:10665/38182
 . World Health Organization technical report series; no. 753.
. World Health Organization technical report series; no. 753.
- ^ Grimes DA. Intrauterine device and upper-genital-tract infection. Lancet. September 2000, 356 (9234): 1013–1019. PMID 11041414. S2CID 7760222. doi:10.1016/S0140-6736(00)02699-4.
- ^ Teal SB, Turok DK, Chen BA, Kimble T, Olariu AI, Creinin MD. Five-Year Contraceptive Efficacy and Safety of a Levonorgestrel 52-mg Intrauterine System. Obstetrics and Gynecology. January 2019, 133 (1): 63–70. PMC 6319579
 . PMID 30531565. doi:10.1097/AOG.0000000000003034.
. PMID 30531565. doi:10.1097/AOG.0000000000003034.
- ^ Bahamondes L, Hidalgo M, Petta CA, Diaz J, Espejo-Arce X, Monteiro-Dantas C. Enlarged ovarian follicles in users of a levonorgestrel-releasing intrauterine system and contraceptive implant. The Journal of Reproductive Medicine. August 2003, 48 (8): 637–640. PMID 12971147.
- ^ 62.0 62.1 62.2 62.3 62.4 62.5 Mirena. Bayer UK. 11 June 2013 [2015-06-18]. (原始内容存档于2015-06-18).
- ^ Donders GG, Bellen G, Ruban K, Van Bulck B. Short- and long-term influence of the levonorgestrel-releasing intrauterine system (Mirena®) on vaginal microbiota and Candida. Journal of Medical Microbiology. March 2018, 67 (3): 308–313. PMID 29458551. doi:10.1099/jmm.0.000657
 .
.
- ^ Nijhuis JG, Schijf CP, Eskes TK. [The lost IUD: don't look too far for it]. Nederlands Tijdschrift voor Geneeskunde. July 1985, 129 (30): 1409–1410. PMID 3900746.
- ^ Kaplan NR. Letter: Lost IUD. Obstetrics and Gynecology. April 1976, 47 (4): 508–509. PMID 1256735.
- ^ Hormonal Contraceptives, Progestogens Only. International Programme on Chemical Safety. 1999 [2006-10-08]. (原始内容存档于2006-09-28).
- ^ Faculty of Family Planning and Reproductive Health Care Clinical Effectiveness Unit. FFPRHC Guidance (April 2004). The levonorgestrel-releasing intrauterine system (LNG-IUS) in contraception and reproductive health. The Journal of Family Planning and Reproductive Health Care. April 2004, 30 (2): 99–108; quiz 109. PMID 15086994. S2CID 31281104. doi:10.1783/147118904322995474
 .
.
- ^ Wong AY, Tang LC, Chin RK. Levonorgestrel-releasing intrauterine system (Mirena) and Depot medroxyprogesterone acetate (Depoprovera) as long-term maintenance therapy for patients with moderate and severe endometriosis: a randomised controlled trial. The Australian & New Zealand Journal of Obstetrics & Gynaecology. June 2010, 50 (3): 273–279. PMID 20618247. S2CID 22050651. doi:10.1111/j.1479-828X.2010.01152.x.
- ^ Bahamondes MV, Monteiro I, Castro S, Espejo-Arce X, Bahamondes L. Prospective study of the forearm bone mineral density of long-term users of the levonorgestrel-releasing intrauterine system. Human Reproduction. May 2010, 25 (5): 1158–1164. PMID 20185512. doi:10.1093/humrep/deq043
 .
.
- ^ Ortiz ME, Croxatto HB. Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action. Contraception. June 2007, 75 (6 Suppl): S16–S30. PMID 17531610. doi:10.1016/j.contraception.2007.01.020. p. S28:
Conclusions
。Active substances released from the IUD or IUS, together with products derived from the inflammatory reaction present in the luminal fluids of the genital tract, are toxic for spermatozoa and oocytes, preventing the encounter of healthy gametes and the formation of viable embryos. The current data do not indicate that embryos are formed in IUD users at a rate comparable to that of nonusers. The common belief that the usual mechanism of action of IUDs in women is destruction of embryos in the uterus is not supported by empirical evidence. The bulk of the data indicate that interference with the reproductive process after fertilization has taken place is exceptional in the presence of a T-Cu or LNG-IUD and that the usual mechanism by which they prevent pregnancy in women is by preventing fertilization. - ^ ESHRE Capri Workshop Group. Intrauterine devices and intrauterine systems. Human Reproduction Update. May–June 2008, 14 (3): 197–208. PMID 18400840. doi:10.1093/humupd/dmn003
 . 温哥华格式错误 (帮助) p. 199:
. 温哥华格式错误 (帮助) p. 199:Mechanisms of action
Thus, both clinical and experimental evidence suggests that IUDs can prevent and disrupt implantation. It is unlikely, however, that this is the main IUD mode of action, … The best evidence indicates that in IUD users it is unusual for embryos to reach the uterus.
In conclusion, IUDs may exert their contraceptive action at different levels. Potentially, they interfere with sperm function and transport within the uterus and tubes. It is difficult to determine whether fertilization of the oocyte is impaired by these compromised sperm. There is sufficient evidence to suggest that IUDs can prevent and disrupt implantation. The extent to which this interference contributes to its contraceptive action is unknown. The data are scanty and the political consequences of resolving this issue interfere with comprehensive research.
p. 205:
Summary
IUDs that release copper or levonorgestrel are extremely effective contraceptives... Both copper IUDs and levonorgestrel releasing IUSs may interfere with implantation, although this may not be the primary mechanism of action. The devices also create barriers to sperm transport and fertilization, and sensitive assays detect hCG in less than 1% of cycles, indicating that significant prevention must occur before the stage of implantation. - ^ Speroff L, Darney PD. Intrauterine contraception. A clinical guide for contraception 5th. Philadelphia: Lippincott Williams & Wilkins. 2011: 239–280. ISBN 978-1-60831-610-6. pp. 246–247:
Mechanism of action
The contraceptive action of all IUDs is mainly in the intrauterine cavity. Ovulation is not affected, and the IUD is not an abortifacient.58–60 It is currently believed that the mechanism of action for IUDs is the production of an intrauterine environment that is spermicidal.
Nonmedicated IUDs depend for contraception on the general reaction of the uterus to a foreign body. It is believed that this reaction, a sterile inflammatory response, produces tissue injury of a minor degree but sufficient to be spermicidal. Very few, if any, sperm reach the ovum in the fallopian tube.
The progestin-releasing IUD adds the endometrial action of the progestin to the foreign body reaction. The endometrium becomes decidualized with atrophy of the glands.65 The progestin IUD probably has two mechanisms of action: inhibition of implantation and inhibition of sperm capacite journal, penetration, and survival. - ^ Jensen JT, Mishell Jr DR. Family planning: contraception, sterilization, and pregnancy termination.. Lentz GM, Lobo RA, Gershenson DM, Katz VL (编). Comprehensive gynecology. Philadelphia: Mosby Elsevier. 2012: 215–272. ISBN 978-0-323-06986-1. p. 259:
Intrauterine devices
Mechanisms of action
The common belief that the usual mechanism of action of IUDs in women is destruction of embryos in the uterus is not supported by empirical evidence... Because concern over mechanism of action represents a barrier to acceptance of this important and highly effective method for some women and some clinicians, it is important to point out that there is no evidence to suggest that the mechanism of action of IUDs is abortifacient.
The LNG-IUS, like the copper device, has a very low ectopic pregnancy rate. Therefore, fertilization does not occur and its main mechanism of action is also preconceptual. Less inflammation occurs within the uterus of LNG-IUS users, but the potent progestin effect thickens cervical mucus to impede sperm penetration and access to the upper genital track. - ^ 74.0 74.1 Thiery M. Pioneers of the intrauterine device. The European Journal of Contraception & Reproductive Health Care. March 1997, 2 (1): 15–23. PMID 9678105. doi:10.1080/13625189709049930.
- ^ Thiery M. Intrauterine contraception: from silver ring to intrauterine contraceptive implant. European Journal of Obstetrics, Gynecology, and Reproductive Biology. June 2000, 90 (2): 145–152. PMID 10825633. doi:10.1016/s0301-2115(00)00262-1.
- ^ FDA drug approval for Skyla. (原始内容存档于2014-08-13).
- ^ Laitinen K. Bayer. businessfinland.fi. [2021-09-21]. (原始内容存档于2021-09-21) (美国英语).
- ^ 2009 Warning Letters and Untitled Letters to Pharmaceutical Companies. U.S. Food and Drug Administration. [2015-06-18]. (原始内容存档于2015-06-18).
- ^ 79.0 79.1 Bekiempis V. The Courtroom Controversy Behind Popular Contraceptive Mirena. Newsweek. 2014-04-24 [2015-06-18]. (原始内容存档于2015-06-18).
- ^ Budusun S. Thousands of women complain about dangerous complications from Mirena IUD birth control. ABC Cleveland. [2015-06-18]. (原始内容存档于2015-06-18).
- ^ Colla C. Mirena birth control may be causing complications in women. ABC 15 Arizona. 2013-05-21 [2015-06-18]. (原始内容存档于2015-06-18).
- ^ Bekiempis V. The Courtroom Controversy Behind Popular Contraceptive Mirena. Newsweek. 2014-04-24 [2016-11-16]. (原始内容存档于2016-11-15).
- ^ Popular contraceptive device Mirena target of lawsuits in Canada, U.S. CTV. 2014-05-21 [2016-11-16]. (原始内容存档于2016-10-26).
- ^ Blackstone H. When IUDs Go Terribly Wrong. Vice. 2016-05-31 [2016-11-16]. (原始内容存档于2016-11-17).
宫内节育器(俗称"螺旋)。



